Overview
- Interoperability is the process by which health IT enables the secure exchange of health information across platforms and without special efforts on the part of the patient
- Interoperability means your practice can better obtain a 360-degree view of your patients’ medical histories in order to provide the highest quality care
- The Office of the National Coordinator for Health Information Technology (ONC) effectuates the Cures Act
- The ONC sets interoperability standards that continue to evolve year to year in order to keep pace with technological advances
The 21st Century Cures Act may be the most important medical law you’ve never heard of. Unlike well-known statutes such as HIPAA and ERISA, which have been around for decades, the Cures Act has been in effect for less than 10 years. Yet, it contains sweeping provisions that affect broad swaths of the US healthcare system, from mental health parity to substance abuse to Medicaid. But buried deep within the legalese is a critical concept of which medical practice administrators, practitioners, and support staff should be aware.
In this post, we’ll provide you with a brief overview of interoperability, as well as the federal government office responsible for setting interoperability standards under the Cures Act.
What is interoperability?
What does interoperability of health records mean? Under the Cures Act, interoperability means health information technology (IT) that:
- “(A) enables the secure exchange of electronic health information with, and use of electronic health information from, other health information technology without special effort on the part of the user;
- (B) allows for complete access, exchange, and use of all electronically accessible health information for authorized use under applicable State or Federal law; and
- (C) does not constitute information blocking.”
One way to think about interoperability is in the context of software we use everyday. Have you ever tried to open an Adobe PDF in Google Drive, only to find out that you need a third-party application to read it? This is an example of 2 technology platforms that do not directly communicate with each other.
Now, imagine you’re a patient who requires treatment from multiple specialists within different offices, each of which uses a different combination of digital and perhaps even paper records. Your complete health record may be hard or even impossible to assemble.
This concept of a patchwork quilt of medical records has been a thorn in the side of patients, advocates, providers, insurance companies, and many others who require access to healthcare information housed within multiple diffuse databases, offices, and technology platforms. The Cures Act, with its focus on interoperability, seeks to change this reality.
The ONC and its Certified Health IT Product List (“CHPL”)
The Office of the National Coordinator for Health Information Technology (ONC) is the federal government office responsible for effectuating the Cures Act by setting standards and rulemaking, including rules that address interoperability. The ONC promulgated the Cures Act Final Rule to provide guidance to those entities impacted by the Cures Act and to clarify their compliance obligations, including around interoperability.
“The ONC publishes a Certified Health IT Product List (CHPL) that you can search to ensure your health IT vendors are up to date in their compliance obligations under the Cures Act.”
One way that the ONC ensures its standards are met is through the ONC Health IT Certification Program. Launched in 2010, the certification program is a voluntary third-party conformity assessment program for health IT products based on the principles found within well-established, standardized frameworks.
The ONC publishes a Certified Health IT Product List (CHPL) that you can search to ensure your health IT vendors are up to date in their compliance obligations under the Cures Act, which include adopting interoperability standards and best practices. The Kareo EHR, a Tebra product, was recently re-certified under the leadership of Beth Onofri and our product team.
The United States Core Data for Interoperability
As part of its certification program, the ONC requires the adoption of the United States Core Data for Interoperability (USCDI). According to the ONC, the USCDI is “a standardized set of health data classes and constituent data elements, including clinical notes, allergies and intolerances, laboratory test results, and medications for nationwide, interoperable health information exchange.”
“The USCDI is “a standardized set of health data classes and constituent data elements, including clinical notes, allergies and intolerances, laboratory test results, and medications for nationwide, interoperable health information exchange.”
The Interoperability Standards Advisory
Another way the ONC promotes interoperability standards is via the Interoperability Standards Advisory (“ISA”). Like the USCDI, interoperability standards must continue to evolve in order to be useful in light of technological and software innovation.
According to the ONC, the ISA is the model by which the ONC “coordinates the identification, assessment, and public awareness of interoperability standards and implementation specifications that can be used by the healthcare industry to address specific interoperability needs including, but not limited to, interoperability for clinical, public health, research and administrative purposes.”
In other words, it represents the ONC’s ongoing efforts to ensure the standards it sets reflect the realities of its stakeholders. The ISA receives frequent updates based on public comments.
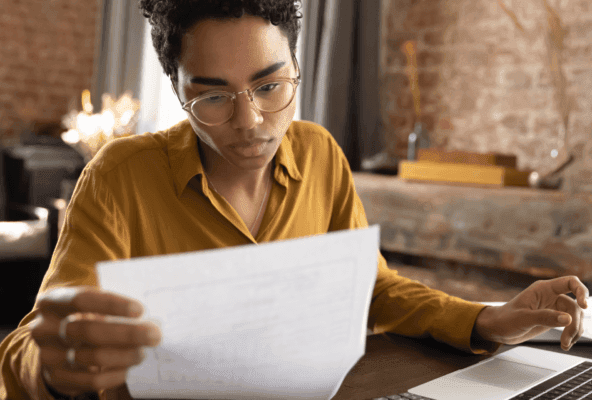
Ensure your software vendors are compliant
Your practice can utilize the Certified Health IT Product List (CHPL) to ensure your software vendors are compliant with the latest health IT standards.
You might also be interested in
Learn how to create a seamless patient experience that increases loyalty and reduces churn, while providing personalized care that drives practice growth in Tebra’s free guide to optimizing your practice.