Overview
- 85% of surveyed healthcare providers believe more patient interaction time would enhance health outcomes.
- Providers spend nearly as much time on EHR documentation as they do with patients, highlighting a significant administrative burden.
- Efficient EHR systems and streamlined administrative tasks are essential for maximizing patient interaction time and improving care quality.
Are you spending enough time with your patients?
According to a recent Tebra survey of over 100 independent healthcare providers — including primary care physicians, psychiatrists, nurse practitioners, and specialists — 85% believe that increasing patient interaction time would positively impact health outcomes. Moreover, 56% of primary care providers wish they could spend less time on electronic health record (EHR) documentation and more time on patient care.

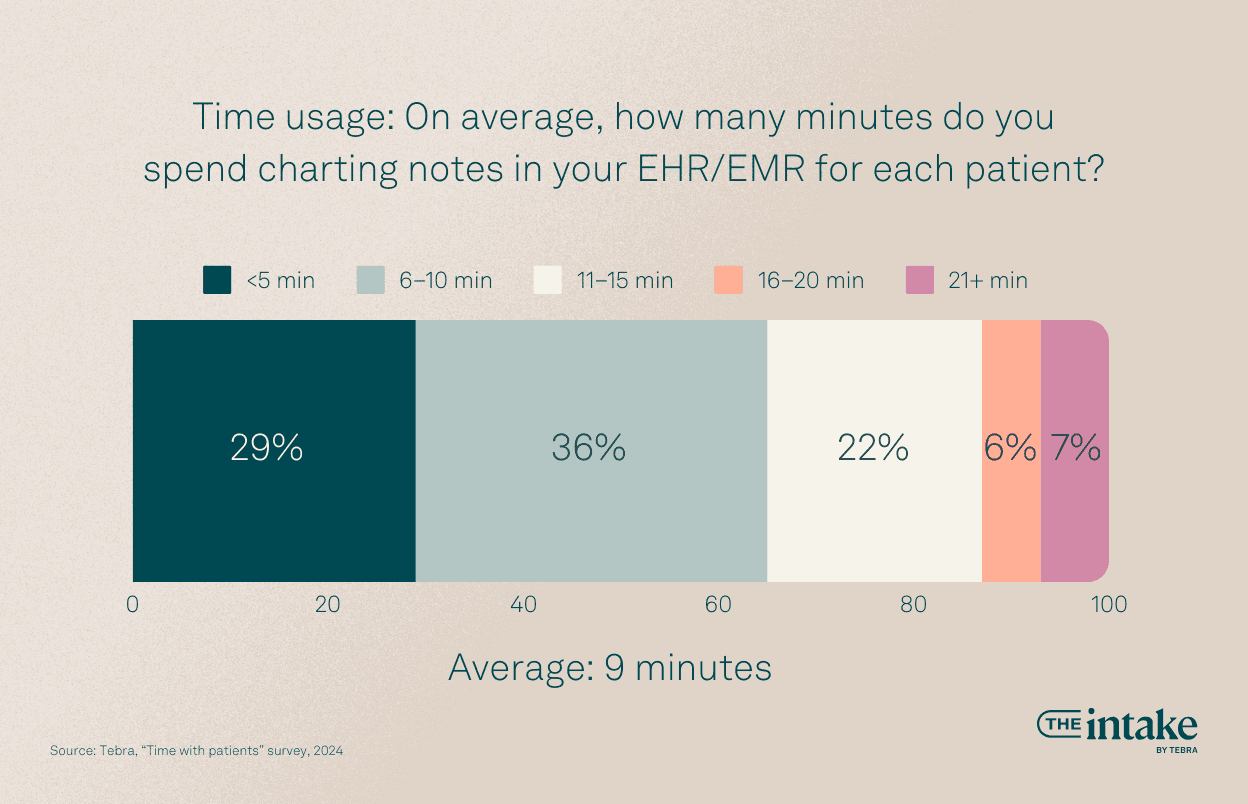
In fact, the survey found that, on average, healthcare providers spend approximately 9 minutes charting notes in their EHR/EMR for each patient, and an average appointment lasts about 15 minutes. Providers wish they could spend more time with patients, reflecting the sentiment that better patient interaction would lead to improved health outcomes.
In today’s complex healthcare landscape, providers face numerous challenges, from intricate billing operations to patient communications and maintaining compliant documentation. These tasks can interfere with the quality of care and overall practice success.
Tebra’s survey highlights a key differentiator for independent healthcare providers: the value placed on patient interactions. The survey also reveals how providers use their EHR software and how to optimize patient interaction time.
This article will cover the report's key findings and explore strategies for maximizing patient interaction time through more efficient EHR usage and streamlined administrative processes.
Download your free resource now
Access it instantly — just complete the form

The current state of patient interactions
Tebra’s recent survey of independent healthcare providers reveals significant variations in the number of patients seen daily across different specialties.
42% of survey respondents see more than 21 patients per day, with primary care physicians and specialists seeing the most patients.

Patient interaction times also have trends based on the provider’s gender. Women providers are more likely to spend more time with patients compared to men providers. With new patients, 70% of women providers spend more than 20 minutes, compared to only 50% of their men counterparts. This pattern holds for returning patients, with 30% of women spending more than 20 minutes, compared to 14% of men. (The survey provided the gender options “woman,” “man,” or “prefer not to answer.”)

Despite these variations, one thing is clear: time spent with patients is declining. Independent healthcare providers face numerous challenges, including administrative burdens and EHR documentation, which impact patient interaction quality and quantity.




Are doctors spending less time with patients?
Physicians are committed to patient well-being, but time management has become a critical pain point. According to our survey, 16% of providers report that their time with patients has decreased over the past year, with pediatric and family medicine doctors declining the most.

One contributing factor is the range of non-clinical tasks that providers must handle. About 27% of primary care providers stated they spend half of their time on tasks unrelated to patient care.
Running a clinic takes a considerable amount of time away from patient health. Even if you have a front desk assistant, providers can still find themselves fielding appointment calls; stuck on hold with insurance companies over prior authorizations or general queries; and devoting time to marketing, billing, and other operational tasks.
“16% of providers report that their time with patients has decreased over the past year.”
All of these items cut into time spent building sound relationships with patients — not to mention getting enough time to learn about their ailments.
The impact of administrative burdens: Are EHRs to blame?
Ever-evolving regulations and complex billing structures demand significant time. Our survey found that 24% of providers spend 5–10 hours weekly on billing and payment processes alone. Verifying insurance and pre-authorizations are among the most time-consuming tasks.

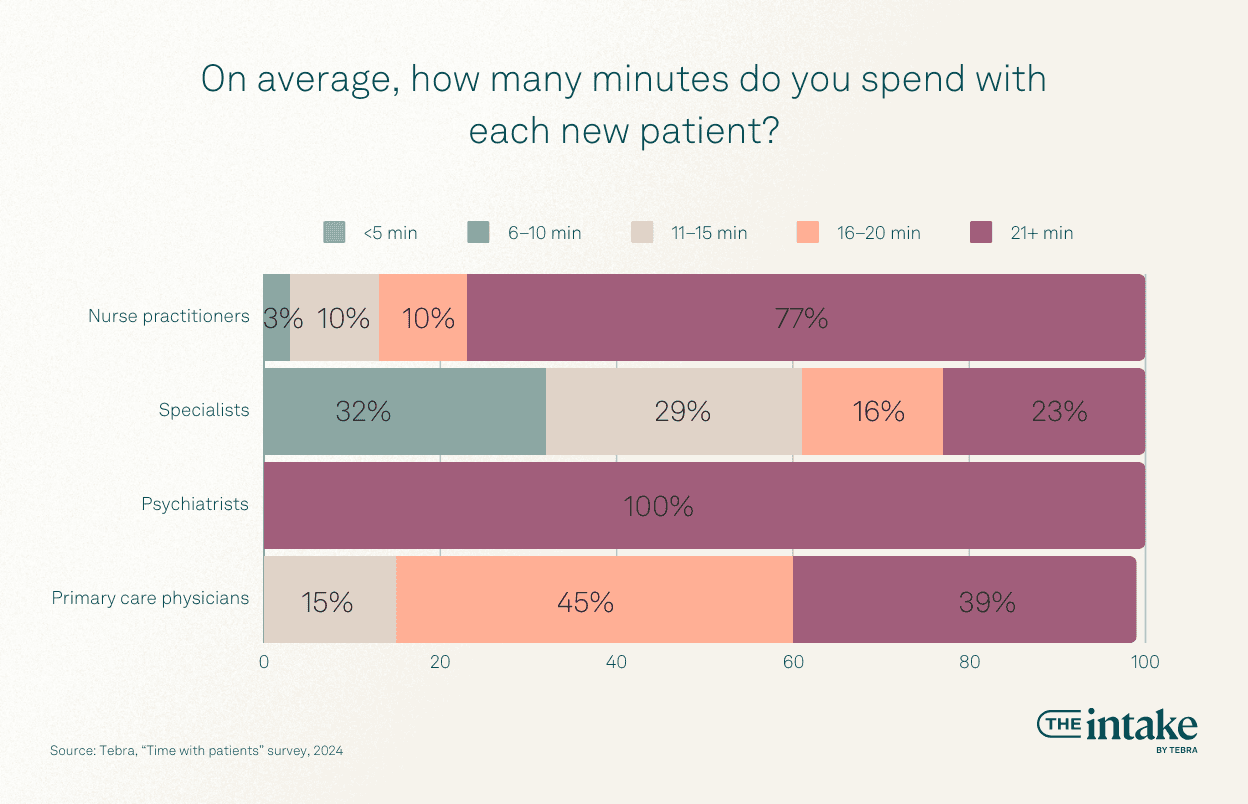
EHRs are pivotal in these interactions, from record keeping to billing. Among primary care providers, 45% reported spending 11–15 minutes with returning patients, and 57% said they spent 6–15 minutes making notes in their EHR. This means that for every minute spent with a patient, providers spend nearly a minute on documentation.
The amount spent on EHR documentation varies by specialty.
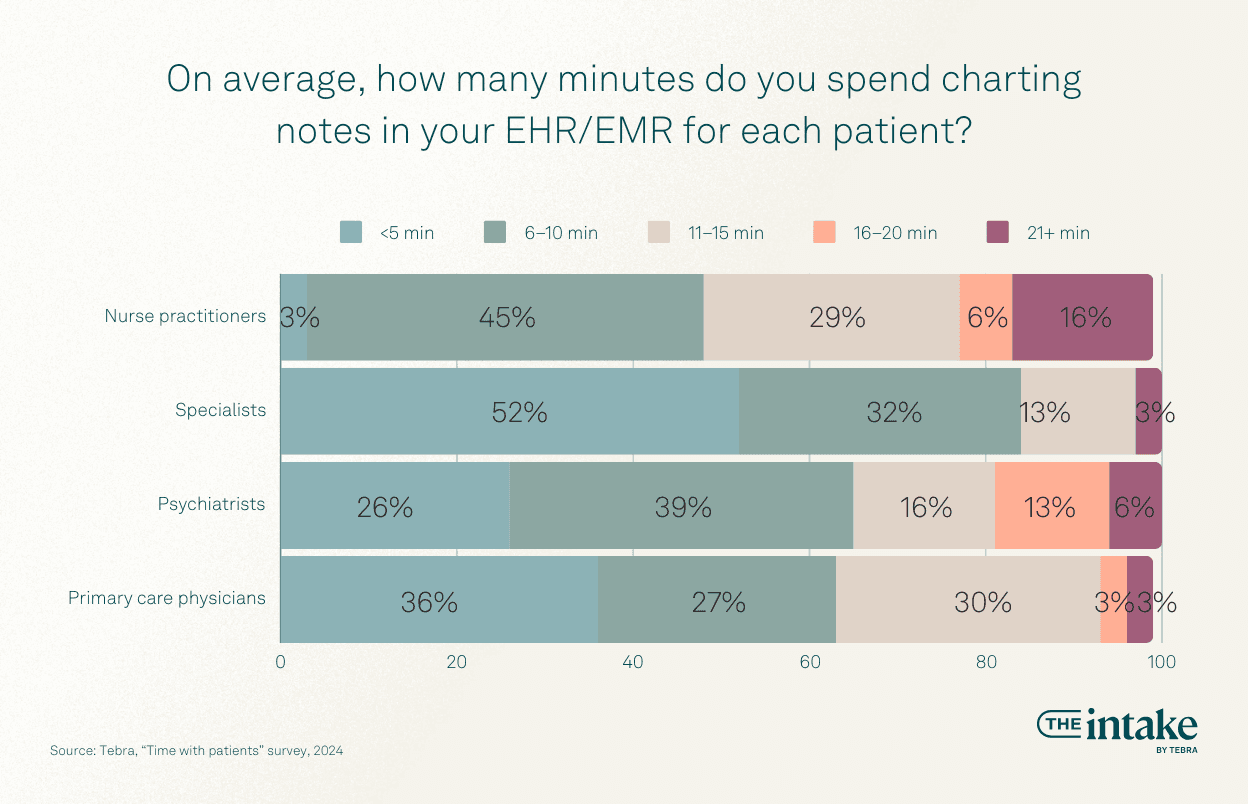
21% of providers spend as much time on EHR documentation as on patient care. Moreover, 1 out of 5 said that they spend more time on documentation than with their patients.

This raises a critical question: is EHR the problem?
It may appear counterintuitive — after all, EHRs are meant to streamline and standardize patient records, reducing errors and administrative time.
However, 52% of providers said their EHR software reduced patient interaction time. Over half said they wanted to spend less time with their EHR and more time with patients.

Furthermore, 54% say that the time spent on EHR documentation outweighs its benefits for patient care.
The EHR isn’t necessarily at fault.
Many issues relate to how the EHR is implemented. A poorly integrated or mapped EHR system significant friction in the patient care process, from appointment booking to care delivery and billing. Overly complex systems are challenging for patients, providers, and practice managers, leading to delays and miscommunication.
Another common EHR hurdle is poor usability, which leads to navigation difficulties and often to errors. EHR training is also a critical component of success — insufficient training can slow down providers.
In short, require efficient and user-friendly EHR solutions.
The importance of provider-patient relationships
Time with patients also links to a key metric that is challenging to quantify: patient relationships.
Patient appointments are rarely focused solely on medical questions. Providers and patients benefit from a solid relationship built on trust and appreciation. Not only can providers offer better care, but they experience improved job satisfaction and a better reputation. However, this is almost impossible to nurture without spending time together.

Over 80% of providers reported time with patients as a key value of their independent practice. This focus differentiates them from corporations and large hospitals, which often minimize patient time. 85% believe that spending time with patients positively affects patient outcomes.
At the same time, 22% of providers are unsatisfied with the time spent with patients. Many barriers prevent them from establishing strong bonds and long-term patient relationships.

Studies have found that successful provider-patient relationships are built on trust, knowledge, respect, and communication. In particular, friction in the communication workflow can break down these elements.
Other barriers to spending more time with patients
Your EHR is not the only barrier to efficient patient visits — communication barriers, such as cultural differences and the need for adaptive interpersonal skills, can create friction in the patient communication workflow.
There are 2 considerable roadblocks to improving provider-patient appointments and relationships:
- Overrunning appointments
- Time-consuming administrative tasks
Overrunning appointments
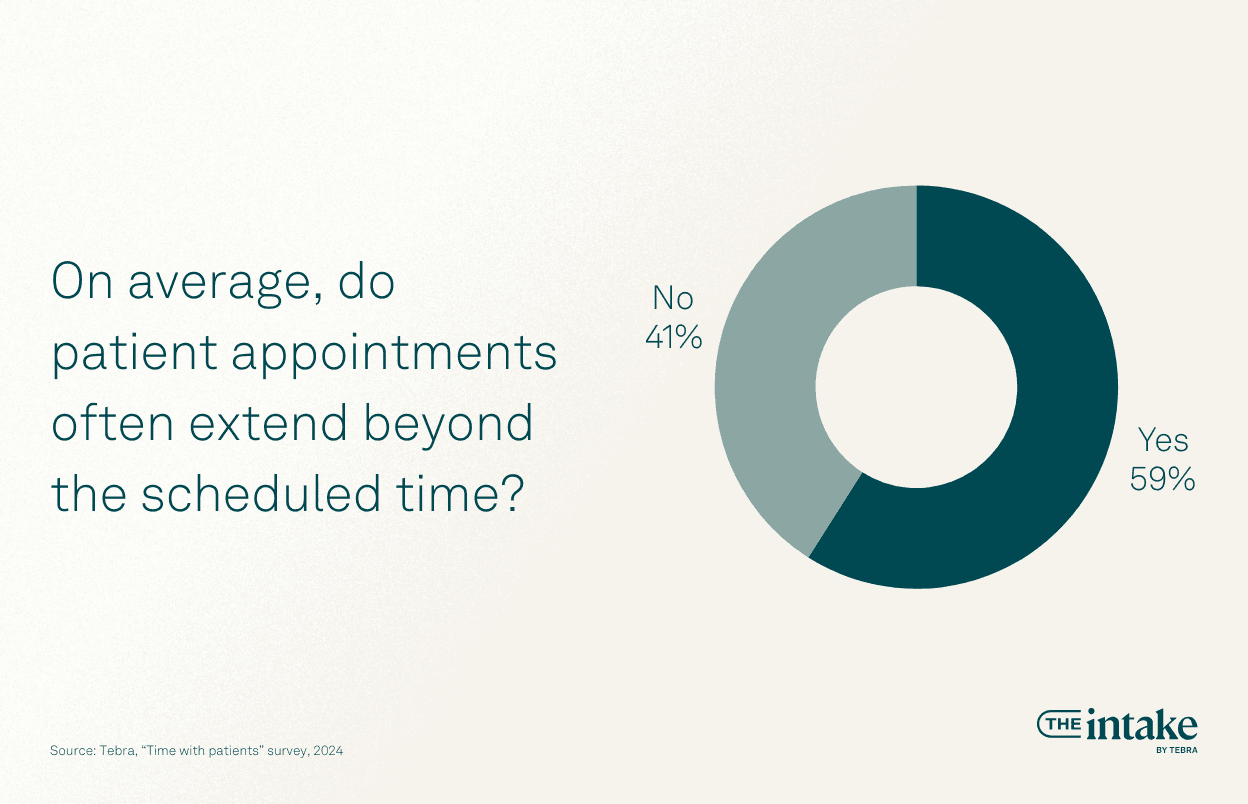
One way to earn trust is to maintain appointment times. Overrunning appointments creates frustration and mistrust for patients and adds pressure on physicians. However, 59% of providers said the average patient visit extends beyond the allotted time frame.
Patient appointments may run over for several reasons, including:
- Patient questions (85%)
- Late arrivals (69%)
- Incomplete information (53%)

When appointments run long, it creates a domino effect where everything gets pushed back. Providers become rushed, the office staff may be overwhelmed with administrative tasks, and important documentation can be neglected.
Time-consuming tasks
Time-consuming administrative tasks also hinder provider-patient relationships. Across all specialties, documentation and charting notes are reported as the most time-consuming tasks, followed by patient communication.
“82% of survey respondents said charting and documentation was the #1 most time-consuming administrative task.”
But how much time do these tasks take?
Let’s consider calendar management. Almost a quarter of respondents said they spend 3 to 5 hours every week just managing the calendar, and 13% said they spend more than 5 hours.
Another 30% reported spending 1 to 2 hours weekly on their Google Business Profile.
Various administrative inefficiencies prevent providers from spending the necessary time with patients. However, there are ways to boost patient interaction time.
Providers generally agree on solutions that could save time during patient communication:
- An effective patient portal
- Easier scheduling tools
- The ability to import patient history
These features in an all-in-one EHR software could significantly improve the patient experience and management.
The impact on providers
72% of survey respondents said spending more quality time with their patients directly contributes to their job satisfaction, but 31% of providers have experienced lower job satisfaction year over year.

Short consultations with patients lead to a number of challenges. These can include errors in case handling, misdiagnoses, and fewer physical examinations.
One reason for this lack of face-to-face time with patients is that providers are seeing significantly more people at a time. This, in turn, contributes to provider burnout. Of providers, 82% reported feeling exhausted, fatigued, or burned out during patient appointments. This is up 2% from an unpublished Tebra survey conducted last year.

These factors contribute to a weaker provider-patient relationship, leading to mistrust and further friction in providing care.
Solutions to maximize time with patients
For some providers, EHR software takes time away from providing care. But that doesn’t need to be the case.
Research has shown several benefits to EHR. For example, a study in Informatics for Health and Social Care found that patient access to EHR reduced costs, improved care, and emphasized patient-centric outcomes. These systems improve healthcare delivery through centralizing patient data and ensuring provider compliance. An efficient EHR system also gives patients and providers 24/7 access to data for care, research, and review.
The key to such success depends on a few factors.
First, a practice must identify an EHR that is as easy to use as it is affordable. Integrating complex software, especially without training, deters physicians and the back office from using it. It also slows down workflows.
To find the best EHR for your practice, you must often invest in mapping out processes and educating your patients. For example, aim to streamline your administrative process by simplifying billing and payment workflows. You may also decide to delegate some administrative tasks to support staff, whether that be in-house office employees or contractors.
What could an optimized EHR look like? Some key features could include:
- Intuitive interface
- Seamless patient record management
- Secure messaging
- Interoperability and integration
- Scalability
- Specialty-specific customization
Another critical consideration is digitizing intake and scheduling.
A sound patient intake, such as a patient portal for pre-visit questionnaires and early communication about appointment expectations, can reduce no-shows and late arrivals.
Once these elements are in place, it’s possible to implement an efficient scheduling system. Efficient scheduling often means offering options, such as phone and online booking calendars.
Then, implement appointment reminders through text messaging or email. On the provider end, these programs should be integrated to reduce double booking, appointment errors, and similar inefficiencies.
Leverage your EHR for a better patient experience
Billing, scheduling, and EHR documentation can be barriers to positive patient outcomes, or they can become accelerators. These tasks are often time-consuming, but with intuitive EHR software that efficiently integrates all of these components, providers can spend less time tinkering with records and more with patients.
Tebra supplies providers with a modern, cloud-based EHR that matches electronic records, electronic prescriptions, electronic labs, and telehealth options with other key practice management features such as:
- Online scheduling
- Automated appointment reminders
- Patient intake
- Text messaging
- A patient portal
- Insurance eligibility
- Claim submissions
- Patient statements
- Revenue analysis
- Practice websites and reputation management
Discover how Tebra can help your practice grow, and schedule a demo with our expert team today.
Methodology
The survey conducted by Tebra aimed to gather insights from independent healthcare providers regarding the time they spend with patients and the challenges they face, particularly related to administrative burdens and EHR usage. It was administered to a sample of 127 independent healthcare providers, encompassing a variety of specialties and roles within their practices. The survey ran from May 9 to 18, 2024. The survey results were not were not weighted. The respondents comprised a diverse group of independent healthcare providers, including 26% in primary care, 25% specialists, 25% nurse practitioners, and 24% mental health physicians. The majority of respondents were practitioners with an ownership stake in their practice (64%), while 35% were practitioners without an ownership stake.
Fair use statement
Feel free to share this article — we ask that you do so for noncommercial purposes and link back to this page.
You might also be interested in
Learn how to create a seamless patient experience that increases loyalty and reduces churn, while providing personalized care that drives practice growth in Tebra’s free guide to optimizing your practice.







