- CY 2026 final rule revises reimbursement, payment rates, and billing policies in the Medicare Physician Fee Schedule.
- Practices and providers should review changes, adjust documentation, and update workflows to protect physician payment.
- Understanding updates supports accurate coding, better patient care, and timely Medicare payments.
Medicare billing changes are the yearly updates to the Medicare Physician Fee Schedule (PFS) that adjust codes, coverage, and payment policies. Details shift each calendar year, often through new or revised Healthcare Common Procedure Coding System (HCPCS) and Current Procedural Terminology (CPT) entries.
For the most current guidance, review Centers for Medicare & Medicaid Services (CMS) materials on the PFS final rule and confirm nuances with your professional organizations. You can also check the CY 2026 PFS final rule fact sheet for a concise overview.
The CY 2026 final rule changes how providers bill and get paid under Medicare Part B. CMS finalized policies affecting caregiver training, cardiovascular risk services, advanced primary care management, telehealth, and E/M complexity, alongside rate-setting updates like the conversion factor.
The focus is practical. Align processes with CMS rulemaking, apply new billing codes correctly, and connect each update to everyday patient care so teams document well and safeguard reimbursement and Medicare payments.
Below, we outline 7 key changes that medical practices and their partnering medical billing companies should consider.
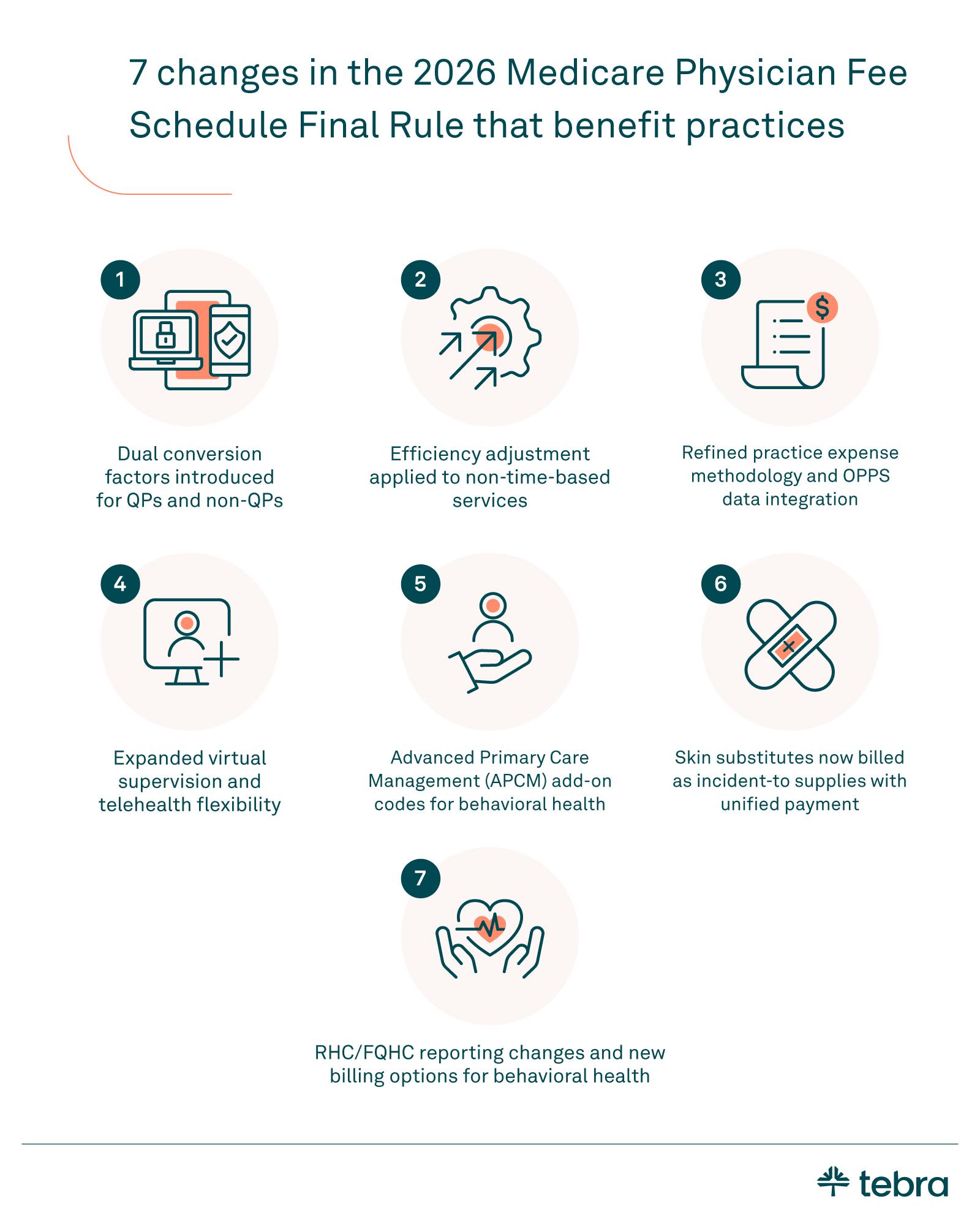
What's new in CY 2026 at a glance
The CY 2026 PFS final rule introduces 7 updates that affect access, documentation, and revenue for clinicians serving Medicare beneficiaries.
- Conversion factor updates: Two conversion factor paths begin — Qualifying Participants (QPs) in Alternative Payment Models (APMs) get +0.75% and non-QPs get +0.25%, with statutory and relative value unit (RVU) adjustments shaping payment rates under the PFS.
- Efficiency adjustment: A −2.5% efficiency adjustment applies to non-time-based services (E/M and care management excluded), refining relative value units and improving pricing methodology.
- Telehealth and supervision: CMS streamlines the Medicare telehealth services list, removes select frequency limits, and allows virtual direct supervision via real-time audio-video (not audio-only). Teaching-physician virtual presence is finalized for qualifying scenarios.
- Primary and behavioral care: Advanced Primary Care Management (APCM) base codes gain optional add-on G-codes for behavioral health services, such as Behavioral Health Integration (BHI) or the Collaborative Care Model (CoCM). Digital mental health device coverage expands (e.g., ADHD). Skin substitutes shift to incident-to-supply payment with a unified rate. Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs) get aligned care management services and reporting updates.
Below, we'll take a look at these changes in more detail, including how they affect medical practices.
1. Dual conversion factors for 2026
Beginning in the calendar year 2026, the PFS uses two conversion factor values rather than one. Qualifying APM participants receive $33.57 with a +3.77% update. Non-QPs use $33.40 with a +3.26% update.
These updates combine the statutory +2.50% increase with about +0.49% tied to finalized changes in work RVUs. CMS also finalized updates to GPCIs and malpractice RVUs, which are reflected in locality payment rates. The practical step for clinicians is to confirm QP status, refresh internal fee schedules, and reconcile expected payment amounts against remits in Q1.
Review how local adjustments and the new methodology interact with your mix of services, since small shifts in RVUs can change physician payment at the code level. Standardize these updates in your EHR software so coding, billing, and reporting match what the Medicare Administrative Contractors (MAC) pay under Medicare Part B.
2. Efficiency adjustment applied to non-time-based services
For CY 2026, CMS finalized an efficiency adjustment of 2.5% to the work relative value units and the intraservice time assumptions for non-time-based services. The policy refines the methodology that underpins the PFS payment system.
It excludes time-based codes such as evaluation and management, care management services, behavioral health services, services on the Medicare telehealth list, and maternity codes with an MMM global period. CMS also updated the exemption list after public comment.
Why does it matter for operations? The adjustment can change code values and payment amounts across specialties. Refresh RVU tables, recalculate locality payment rates, and compare modeled results to early remittances. Pay close attention to procedures that rely on historic time surveys, since small RVU shifts can move totals in either direction.
Update charge masters and fee schedules, then audit the first month of 2026 claims for variance. Align finance, coding, and compliance teams so policy updates and payer processing match.
3. Practice expense methodology updates and OPPS data use
For 2026, CMS refined practice expense valuation to better reflect practice cost differences between office and facility settings. The final methodology recognizes higher indirect costs for office-based care compared to facility care, which can shift practice expense RVUs and, in turn, payment rates.
CMS also began using selected Outpatient Prospective Payment System (OPPS) data to inform relative rates for certain technical services, starting with radiation treatment and some remote monitoring, which supports more predictable pricing across settings.
What this means for operations: Review any codes in your mix that rely heavily on practice expense inputs. Model the impact on payment amounts for common procedures in both office and hospital outpatient department contexts.
Update fee schedules, check your payer mappings, and compare expected totals to your first-quarter remittances. Align finance and coding so charge descriptions and Place of Service choices match how services are furnished, since the facility versus non-facility split now matters even more for forecasting.
4. Telehealth and supervision updates
CMS simplified how services get onto the Medicare telehealth services list, which should shorten the path from code request to coverage. The agency also removed long-standing frequency limits for subsequent inpatient, subsequent nursing facility, and critical care consults furnished by telehealth.
For supervision, physicians can now meet direct supervision requirements through real-time two-way audio-video telecommunications when appropriate. Audio-only does not satisfy virtual supervision.
It still applies when the underlying service can be furnished via audio-only, and documentation must reflect why video was not feasible. Teaching settings received a permanent update as well. A teaching physician may be virtually present when the service itself is furnished virtually.
Teams should confirm local MAC guidance, record modality and location, and align billing for physician services with in-person availability rules. Update intake prompts to capture consent and modality, and adjust EHR smart phrases so the note clearly shows audio-video or audio-only and any required modifiers.
5. Behavioral health and APCM add-ons
CY 2026 introduces add-on code options that let practices pair APCM with behavioral health services such as BHI or the CoCM. In practical terms, you can report APCM for ongoing primary care management, then layer the appropriate behavioral health service when the care plan requires it.
This supports stepped-care interventions, smoother handoffs, and clearer documentation for team-based treatment. CMS also expanded coverage for digital mental health treatment devices to include ADHD, which can complement screening, titration check-ins, and follow-up inside primary care.
Align care plans, note who is directing treatment, and verify that billing combinations don't duplicate work on the same day. Update templates in your EHR software so problem lists, screening results, and follow-ups map cleanly to the selected codes.
6. Skin substitutes: Incident-to supplies with a unified rate
For CY 2026, CMS will pay for skin substitutes as incident-to supplies when applied with a covered procedure under the PFS in non-facility settings and under OPPS in a hospital outpatient department. Categories are aligned to FDA regulatory status, including 361 HCT/P, 510(k) devices, and PMA devices. A single national payment rate of approximately $127.28 applies in 2026, with the intent to differentiate by category in later years.
For practices, confirm local packaging and status indicators, capture product details in the note, and coordinate with supply management so claims reflect the finalized payment policies. If you bill across multiple payment models, keep office and facility workflows separate and verify edits before submission.
7. RHC/FQHC policies and reporting
For supervision, CMS now allows virtual direct supervision through real-time audio-video when required, which can expand patient access in rural settings. Billing for Medicare telehealth services using G2025 remains available, including audio-only encounters when appropriate, through December 31, 2026.
CMS additionally recognizes designated care coordination services for separate payment in RHCs and FQHCs, so align your visit templates, modifiers, and claim edits to avoid overlaps with other billable services. Update intake to capture modality, supervising practitioner presence, and any technology limitations, then audit monthly to confirm correct use of component reporting and telehealth rules.

Where the PFS applies and where it doesn't
Use this quick table to see where the Physician Fee Schedule (PFS) applies and where it does not in Medicare Part B's payment system.
| Physician Fee Schedule applicability by setting and payment method | ||
| Setting or rule | How it's paid | Notes for practices |
| Physician offices and similar Part B settings | Paid under the PFS in a fee-for-service payment system | Claims use CPT/HCPCS. CMS pricing methodology converts RVUs, practice costs, and other factors into payment. In 2026, separate conversion factors apply for QP and non-QP clinicians. |
| In a hospital outpatient department | Paid under OPPS, not the PFS, for the facility component | Professional services by clinicians are still paid under the PFS. Follow facility packaging and status indicators, and verify local policies before scheduling and billing. |
| Diagnostic tests with professional and technical components | Split billing possible | The technical component may be billed by independent diagnostic testing facilities, while the professional component is paid under the PFS. Use correct modifiers and place of service. |
| Rural Health Clinics and Federally Qualified Health Centers | Paid under RHC/FQHC methodologies, not the standard PFS | Some services align with PFS policies. In 2026, APCM add-ons, virtual direct supervision, and telehealth billing rules apply per finalized guidance. Use G2025 for eligible telehealth through December 31, 2026. |
| In Medicare Advantage plans | Often aligned to PFS policy, but governed by contract terms | Check the plan agreement for covered services, effective dates, prior authorization, and payment timing. Policies may lag PFS updates. |
| Governance and roles (CPT vs. CMS) | AMA maintains CPT. CMS sets PFS policy and rates. | Use CPT guidance for code selection and CMS rules for coverage and pricing. Keep code updates and payer bulletins synced in your workflow. |
Quality Payment Program notes
CY 2026 PFS updates interact with the Quality Payment Program. Confirm your participation track in MIPS or an APM, since policy changes can shift quality measures, data submission, and scoring. If you use value pathways tied to primary care or chronic disease, verify the current measure set and benchmarks.
If you're in an ACO, review attribution rules, reporting cadence, and any overlap with care coordination so you don't double-count. Align registry submissions with what your EHR captures, and document exclusions or exceptions in the chart.
Many groups blend fee-for-service billing with alternative payment models. Update policies, templates, and internal audits together. Map new or revised billing codes to the right quality measures and value pathways, track performance during the year, and reconcile results before close to prevent surprises.
Implications for mental and primary care workflows
Here's how the 2026 updates translate into everyday steps for integrated care in primary care settings.
- Integrate screening: Use caregiver training and ASCVD services to embed mental health checks in primary care visits. Route positive screens for timely follow-up and care planning.
- Use hybrid touchpoints: Support adherence, mood tracking, and coordination with brief digital check-ins and APCM G-codes. Schedule in-person visits when clinically needed.
- Match codes to services: Align telehealth encounters, care management, and evaluation visits so virtual touches do not overlap with separately billable services or global periods.
- Document precisely: Capture risk factors, screening tools, time spent, modality, and who participated. Note handoffs to behavioral specialists to keep claims clean and traceable.
- Close the loop: Set reminders for follow-ups, track outcomes, and update plans. Use team huddles to reinforce consistent workflows across sites and clinicians.

Put the 2026 updates to work
For physician practices, the CY 2026 changes are practical steps, not abstractions. Build simple workflows to capture the new billing codes, monitor payment amounts, and document evaluation and management complexity at every visit. Small process checks now can prevent denials later.
Standardize checklists and claims edits in your EHR software so the right fields, codes, and modifiers appear when teams need them. If you want a central place to align scheduling, billing, and reporting, visit Tebra. Tebra's goal is straightforward: help healthcare providers deliver care efficiently while keeping a medical practice financially steady and patient-friendly.
FAQs
Frequently asked questions about Medicare for private practices
Glossary
Understanding the terminology in the 2026 Medicare Physician Fee Schedule Final Rule can help practices apply updates correctly. Below is a reference list of key terms and acronyms.
| Key terms and acronyms in the 2026 Medicare Final Rule | |
| Term/Acronym | Meaning |
| PFS | Physician Fee Schedule for Medicare Part B services. |
| CMS | Centers for Medicare & Medicaid Services sets policy and rates. |
| CPT | The code set maintained by the AMA is used to report medical services. |
| HCPCS | Code set that includes CPT and additional Medicare-specific billing codes. |
| RVU / WRVU | Relative value units. Work RVU is the clinician effort component. |
| Conversion Factor | Dollar amount that converts RVUs into payment amounts. |
| E/M | Evaluation and management visits are reported with CPT codes. |
| G-Codes | Medicare HCPCS codes that start with "G," often for management or tech-enabled services. |
| MIPS | Merit-based Incentive Payment System under the Quality Payment Program. |
| Modifier | Two-character claim suffix used to convey circumstances affecting payment policies. |
| APM | Alternative Payment Model track within QPP for participating clinicians. |
| ACO | Accountable Care Organization. |
| FQHCS / RHCS | Federally Qualified Health Centers and Rural Health Clinics. |
| OPPS | Outpatient Prospective Payment System for hospital outpatient department claims. |
| Medicare Advantage | Private plan option (Part C). Coverage and timing follow plan contracts. |
| MAC | Medicare Administrative Contractor. |
| APCM | Advanced primary care management codes (G0556–G0558). |
You might also be interested in
Crack the code for beating medical billing challenges with this free workbook — which provides tips around improving patient collections, streamlining claims submissions, and reducing rejections and denials.