Efficient patient data management is essential for every medical practice, regardless of size. For small practices, adopting an electronic health record (EHR) or electronic medical record (EMR) system can bring substantial benefits by streamlining operations, improving workflow, and enhancing the quality of care from healthcare providers. The right system empowers practices to maintain a high standard of personalized care while meeting modern expectations for convenience and accessibility.
With features like a patient portal, EHR systems empower small practices to securely share patient information, improve coordination, and deliver better outcomes. Choosing the right EHR software ensures these improvements, supports better patient experiences, and fosters a more sustainable practice.
| Looking for an EHR that won’t slow you down? This free guide helps you find one that supports your care — not your paperwork. |
Understanding EHRs and EMRs for small private practices
The terms "EHR" and "EMR" are often used interchangeably, but they represent different concepts of health information management. Let's dive into the differences to better understand their functionality and how they can support small practices in managing patient information effectively.
Key differences between EHR and EMR systems
While both EMR and EHR systems digitize patient information, they serve distinct purposes in a practice.
EMRs are electronic medical records that act as digital versions of patient charts, used primarily within a single practice for diagnoses and treatment plans. In contrast, EHRs are a more comprehensive solution that enables patient data sharing across multiple providers and healthcare settings.
This interoperability supports better care coordination, continuity of care, and enhanced patient engagement. This distinction is important for small practices to consider when selecting the best EHR software for their needs, as the right system can streamline workflows, improve quality care, and ensure compliance with HIPAA regulations.

| EMRs (electronic medical records systems) | EHRs (electronic health records systems) |
| Digital charting for a single practice | Comprehensive and integrated records |
| Limited accessibility | Interoperability across facilities |
| Single-practice application | Enhanced care coordination |
| Continuity of care |
EMRs offer:
- Digital charting for a single practice: EMRs consolidate patient information within one office, providing provider-specific documentation that includes physician notes, treatment plans, and prescription details.
- Limited accessibility: EMRs are typically stored locally, which restricts data sharing with other healthcare providers.
- Single-practice application: Designed for use within a single facility, EMRs are ideal for practitioners who work privately or in smaller settings.
Meanwhile, EHRs offer:
- Comprehensive and integrated records: EHRs consolidate patient data from multiple providers, creating a detailed medical history along with administrative and billing information.
- Interoperability across facilities: EHRs allow authorized users to share data across labs, imaging centers, pharmacies, and other care settings, enabling better care coordination and consultations.
- Enhanced care coordination: By providing a complete view of a patient's medical journey, EHRs reduce duplicate tests, missed diagnoses, and errors in medical billing.
- Continuity of care: Unlike EMRs, EHRs follow patients across different care settings, supporting communication between healthcare providers and enhancing patient safety.
Benefits of EHRs for private practices
For small private practices, adopting an EHR or EMR system can offer a range of benefits for both providers and patients. EHR systems consolidate critical health information into an all-in-one solution, streamlining operations and enabling better patient care. Cloud-based EHR platforms make it easier for private practices to securely manage patient records while improving efficiency and outcomes.
Improving patient care
EHRs for small practices allow them to securely share patient data with other providers, supporting better care coordination for patients needing specialized treatment or hospitalization. This interoperability ensures a seamless patient experience and fosters higher-quality care.
EHRs provide real-time access to comprehensive patient records, which helps providers make informed decisions, avoid duplicate testing, and reduce errors. Standardized templates and checklists further support accurate and consistent documentation. Key features such as telemedicine capabilities and advanced practice management software allow small practices to improve efficiency and enhance care delivery.
Streamlining administrative tasks
EHRs and EMRs simplify administrative tasks by automating scheduling, billing, and documentation. With customizable templates, practices can optimize workflows to meet their unique needs, ensuring meaningful use and higher usability. Real-time access to digital patient records reduces administrative burdens, allowing providers to focus on patient care rather than paperwork.
By supporting care coordination and improving operational efficiency, EHR systems deliver high-quality results while meeting the demands of small practices.
Maximizing revenue
EHRs help small practices improve their financial health by streamlining billing processes, auto-populating claim forms, and reducing errors to minimize claim rejections. This ensures timely reimbursements from Medicare and private insurers while boosting cash flow.
Modern EHR systems also provide real-time insights into revenue cycle performance, helping practices make data-driven decisions about their operations. With integrated financial tools and predictable pricing models, practices can better forecast and manage costs while maintaining their private practice status.
Additionally, features like EMR software and referral management improve ease of use, creating new opportunities for practice growth without adding administrative burden.

Pros and cons of EHRs and EMRs
While EHRs and EMRs offer clear advantages for small practices, it’s important to balance the benefits with the potential challenges. The table below highlights the most common pros and cons of adopting an EHR, helping practice leaders weigh both the operational gains and the practical considerations before making a decision.
| Pros | Cons |
| Improves patient care with real-time access to comprehensive records | High upfront and ongoing costs (software, hardware, training) |
| Streamlines administrative tasks like scheduling, billing, and documentation | Potential workflow disruptions during transition |
| Enhances revenue cycle management with fewer errors and faster reimbursements | Staff resistance or slow user adoption due to learning curve |
| Strengthens care coordination through data sharing and interoperability | Data migration challenges from legacy systems |
| Supports compliance with HIPAA and other regulations | Dependence on vendor support and system updates |
Tips for evaluating EHRs
Small private practices face tight budgets, limited resources, and the pressure to deliver high-quality care. The best EMR/EHR for private practice can help overcome all of these challenges and more.
Features to consider
When evaluating EHR systems for your small practice, it's important to focus on features that enhance efficiency and improve patient care. Advanced functionalities can streamline operations and optimize your practice's workflow.
Key features to look for include:
- Appointment scheduling to manage patient visits efficiently
- ePrescribing to simplify medication management
- Telehealth integration for offering remote consultations
- Messaging tools to enhance communication between providers and patients
- Medical billing support to reduce errors and maximize reimbursements
- Customizable templates tailored to your practice's specific needs
- Patient engagement tools like portals for secure communication and access to records
- Seamless data sharing to ensure interoperability with other providers and facilities
- Automation to lighten the burden of repetitive manual tasks
- Modular tools you can add as your practice grows
- Regulatory compliance, including meeting interoperability standards
Choosing a user-friendly EHR system with these advanced features will help your practice deliver high-quality care while optimizing daily operations.
Cost considerations
Cost is a primary consideration for small practices, as EHR implementation can vary widely in expense.
Look beyond the initial EHR costs and evaluate the total cost of ownership, which includes licensing fees, training, ongoing support, and potential upgrade costs. Additionally, consider the implementation process itself; some EHRs offer extensive onboarding support, with guided training and configuration, while others require a more hands-on approach from the practice.
Factoring in the potential impact on daily operations during the implementation phase is essential, as a lengthy or challenging transition can disrupt patient care and workflows. Opt for a system that fits your budget but also provides robust support and minimal downtime during setup.
How to implement EHRs and EMRs in small practices
Selecting the right EHR or EMR is a key decision for small practices, impacting not only daily operations but also long-term success and sustainability. It's not just about functionality but also about finding the right vendor partner who will support you in all aspects of implementation, training, customization, and maintenance.
Choosing the wrong system can lead to costly disruptions, inefficiencies, and dissatisfied staff and patients. The process requires a substantial time commitment, preparation, research, and strategic evaluation of potential systems and vendors.
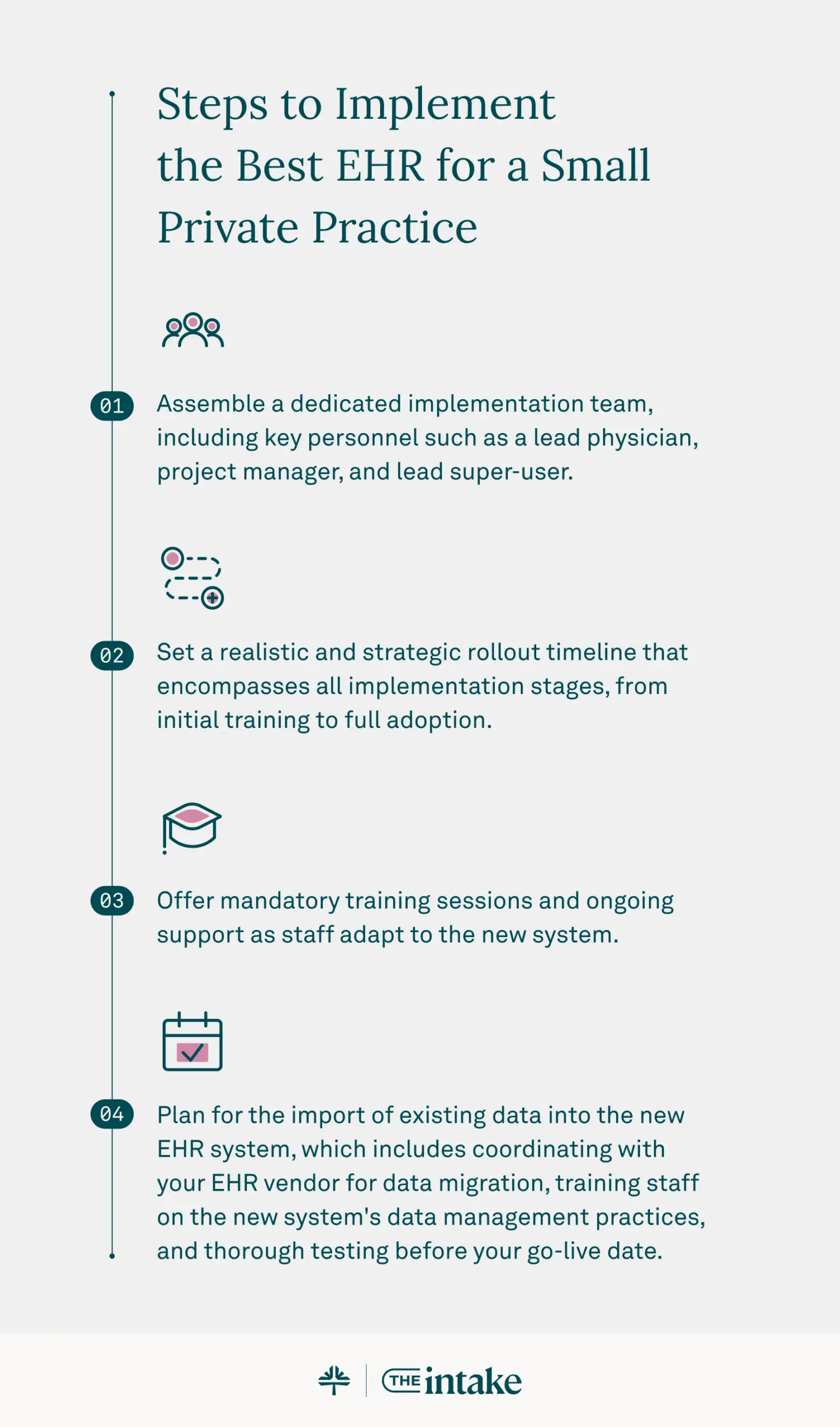
Here are steps you can take to implement the best EHR for a small private practice:
- Assemble a dedicated implementation team, including key personnel such as a lead physician, project manager, and lead super-user.
- Set a realistic and strategic rollout timeline that encompasses all implementation stages, from initial training to full adoption.
- Offer mandatory training sessions and ongoing support as staff adapt to the new system.
- Plan for the import of existing data into the new EHR system, which includes coordinating with your EHR vendor for data migration, training staff on the new system's data management practices, and thorough testing before your go-live date.
| Love content like this? Join thousands of independent providers who receive our weekly newsletter with tips on running a more efficient, profitable practice. Sign up for the newsletter. |
Post-implementation: Measuring the impact
Once the system is fully implemented, it's important to measure its impact on practice efficiency and patient care.
Set benchmarks before implementation to track improvements in areas such as patient wait times, documentation accuracy, billing accuracy, and appointment scheduling. Use the EHR reporting features to monitor these metrics over time, providing insights into how the system has affected productivity and identifying areas for further optimization.
Regularly reviewing and analyzing this data helps assess the return on investment and ensure that the EHR continues to meet practice goals. It can also reveal new opportunities for workflow improvements or additional training needs — making it easier to maintain a high level of efficiency and care quality in the long run.
Frequently asked questions
Here are answers to some of the most common questions small practices have when deciding between an EMR and an EHR.
1. What are 3 benefits to patients and healthcare providers that both EHRs and EMRs offer?
Both digitize charts for instant access, reduce errors with legible notes, and automate tasks like e-prescribing. This means safer care for patients and less administrative work for your staff.
2. What are the benefits of EHR vs EMR?
An EHR’s core benefit is interoperability. It lets you securely share data with labs and specialists for better care coordination. An EMR cannot, limiting data to just your practice.
3. What are the benefits of the electronic medical record system?
An electronic record system replaces paper charts, giving you instant access to patient histories. It streamlines your billing process for faster payments and eliminates physical storage costs.
4. What are the legal benefits of an EMR system?
An EMR creates a time-stamped audit trail, which strengthens your malpractice defense. Its security features improve HIPAA compliance, while customizable templates ensure clear, consistent documentation to reduce legal risk.
Selecting the right small practice EHR
Choosing the right EHR and practice management software for your small practice starts with understanding essential features and carefully considering factors like cost, user-friendliness, and system compatibility. The right EHR system can revolutionize your small practice. Explore Tebra's cloud-based, ONC-certified EHR solutions to simplify workflows, enhance patient care, and support your practice's long-term success.
You might also be interested in
- How EHRs and healthcare technology improve efficiency: See how digital tools can streamline your workflows and reduce day-to-day friction.
- How to identify EHR needs by specialty: Understand what features to look for based on your specialty and patient care model.
- Want to explore a modern EHR built for your needs? Book a free demo and get a guided tour.
- Current Version – Sep 12, 2025Written by: Jean LeeChanges: This article was updated to include the most relevant and up-to-date information available.
- Sep 10, 2025Written by: Ryan YatesChanges: This article was updated to include the most relevant and up-to-date information available.
- Aug 20, 2025Written by: Jean LeeChanges: This article was updated to include the most relevant and up-to-date information available.







