
- Sliding fee scales adjust patient fees based on eligibility, household income, and family size to improve access to care.
- Healthcare providers must define eligibility criteria, set discount tiers, and document compliance to stay audit-ready.
- A clear, consistent policy helps boost patient engagement, ease administrative work, and protect your practice’s financial health.
A sliding fee scale helps people get the healthcare they need when they need it by reducing out-of-pocket costs based on income and family size. It supports uninsured patients and those who have limited health insurance. The sliding fee scale applies across multiple healthcare services and medical settings, including community health centers and private health clinics.
These programs strengthen public health and align with the federal health center program, so more patients can access care at a fair sliding scale fee. This guide outlines how providers and billing staff can assess patient eligibility, collect documentation, and implement sliding fee scale discounts accurately. It also covers where these programs typically apply, the types of services they include, and how to adjust sliding scale determinations when a patient’s financial situation changes.
What is a sliding fee scale?
In the United States, a sliding fee scale is a payment policy that adjusts healthcare costs according to household income and family size. It applies a sliding scale fee so patients pay an amount that matches their income levels.
Most community health centers and every federally qualified health center use a sliding fee discount program guided by the federal poverty guidelines to qualify patients for financial assistance.
Eligible patients can receive care at a health center or health clinic with reduced charges, which supports public health while keeping doors open for those who need it most. Clinics determine the discount after verifying income documentation and reassess their eligibility annually.
Why it matters: Benefits for uninsured and insured patients
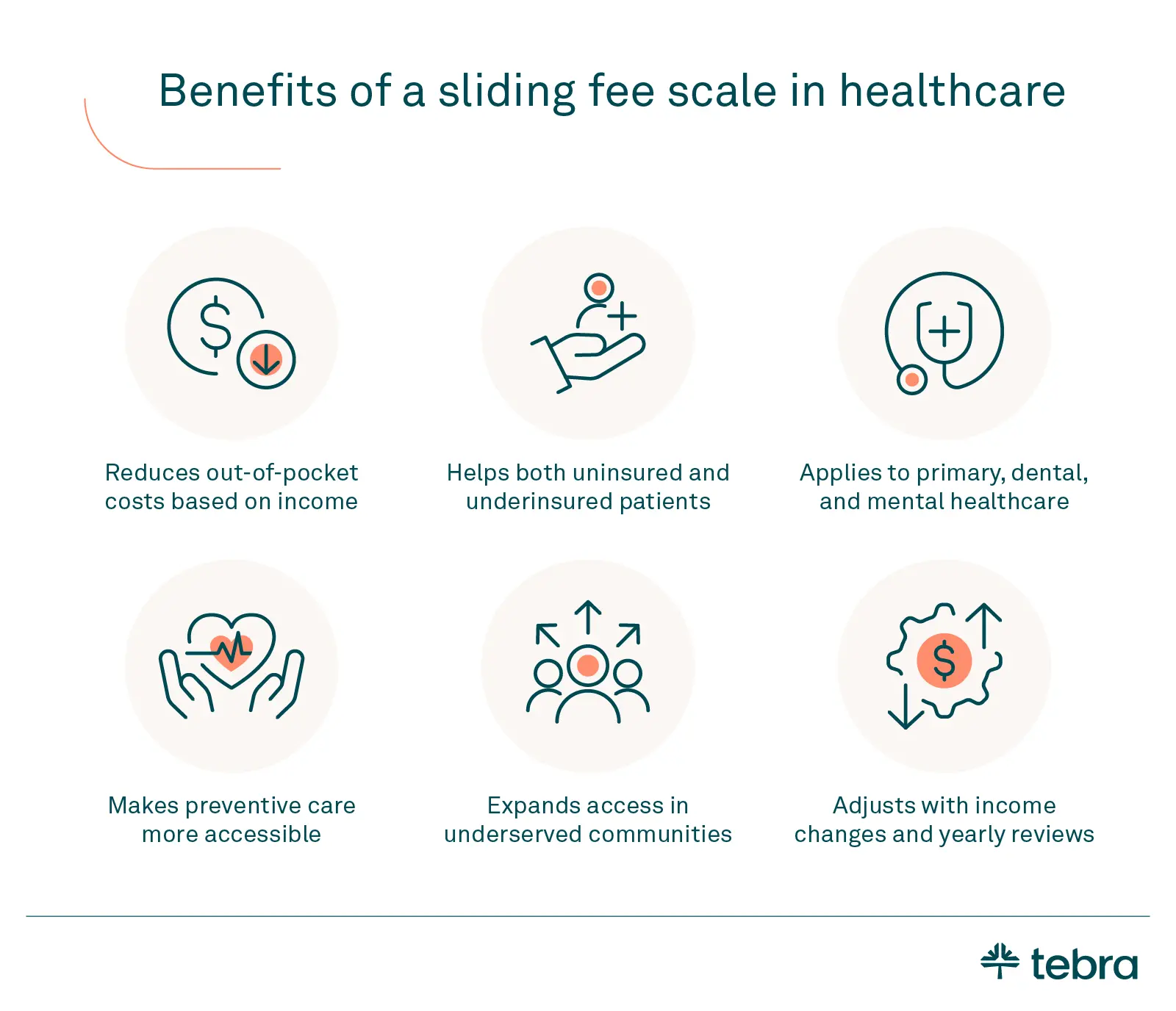
Here's how sliding scales can help uninsured patients and insured patients alike.
Reduced out-of-pocket expenses
Sliding fee scales lower the immediate cost of care by reducing a patient's copay, trimming deductibles, and capping out-of-pocket charges according to income. Clinics review household size and earnings to set fair rates, so people can get treatment sooner with targeted financial assistance rather than delaying appointments or skipping medications.
Broader access to behavioral and dental services
Sliding scales extend beyond primary care. Clinics apply reduced pricing to behavioral health counseling, mental health follow-ups, and dental services such as cleanings, X-rays, and fillings.
Lowering fees across these healthcare services means patients can pursue preventive and ongoing medical care instead of postponing treatment until problems become urgent later.
Support for both uninsured and underinsured
It's a common misconception that sliding scales are only for uninsured patients. However, they also ease costs for insured patients with high deductibles or gaps in their insurance plans. When a clinic uses a sliding fee scale, charges adjust according to income, reducing bills and helping families budget for visits and follow-ups.
Encouraging preventive care
Lower fees make routine visits and screenings realistic. Low costs improve access to medical care, support public health, and reduce avoidable crises that strain clinics, hospitals, and human services programs over time. When costs drop, patients seek healthcare earlier, complete follow-ups, and manage conditions before they worsen.
Equity through community health centers
Sliding fee policies promote equity by bringing affordable care into underserved neighborhoods. Community health centers and each federally qualified health center offer discounts so patients can visit a local health clinic or health center without postponing care. The result is steadier access, better continuity, and fewer preventable emergencies.
Download your free resource now
Access it instantly — just complete the form

Eligibility requirements: Who qualifies?
Eligibility for a clinic's sliding fee scale is based on household size, family size, and annual income compared with the federal poverty level. Clinics use the federal poverty guidelines to calculate a percentage of FPL and then set discounts across income levels. Eligible patients can qualify at a health center when the patient's income and household members meet those thresholds.
Most programs require proof of income. Patients are required to bring in recent pay stubs (no more than 30 days old), a tax return (1040), W-2s, and any Social Security award letters. Documentation of Medicaid or Medicare status typically also helps.
Patients can expect to reapply each year or whenever their income, family size, or address changes so the clinic can keep their discount current.
Types of acceptable proof of income
Clinics verify household income for a sliding fee scale with the following proof of income:
- Tax return (1040): Confirms prior-year annual income and household income and is helpful for setting income levels.
- Pay stubs (last 30 days): Primary evidence of current wages and patient's income.
- W-2 wage and tax statements: Summarize employer earnings and corroborate with the tax return.
- Social Security or disability letters: Document monthly benefits from Social Security programs.
- Medicare or Medicaid documentation: Verifies Medicare or Medicaid eligibility and coverage status.
- Bank statements (when others aren't available): Show regular deposits or benefits.
- Alternative verification (per policy): Employer letter, zero-income self-declaration, self-employment ledger or 1099s, or a letter of support from a shelter or caseworker.
Documentation requirements vary by clinic. Publish accepted documents on patient-facing materials and train front desk staff to explain options.
How sliding fee scales are structured
Most clinics base their sliding fee scale on the updated federal poverty guidelines. Eligibility is calculated as a percentage of the federal poverty level using verified household income and family size. In a health center or federally qualified health center, the sliding fee discount program typically follows this structure:
- At or below 100% FPL: Full discount, or a small minimum fee or nominal fee may apply.
- 101% to 200% FPL: Partial discounts scaled to verified income levels.
- Above 200% FPL: Usually no discount, though other financial assistance may be available.
Minimum fee and nominal fee refer to small out-of-pocket amounts paid by patients in the highest discount tier. These charges help offset administrative costs, are set by board-approved policy, and should not create a barrier to care. Amounts and thresholds vary by clinic policy, payer rules, and state guidance.
Where to find sliding fee scale programs
Most community health centers and every FQHC (Federally Qualified Health Center) offer a sliding fee scale. Programs also appear at some nonprofit clinics and private practice institutions that serve underserved areas.
Eligibility details are posted on a health center or health clinic website, in waiting areas, and within patient health resources. Patients can also ask the front desk, financial assistance counselors, or enrollment navigators for help.
Fees are typically set using income thresholds based on the federal poverty guidelines published by the United States Department of Health and Human Services. Discounts often extend to behavioral health, mental health, and dental services, not just routine healthcare.

The application process
Follow a clear workflow to enroll patients in a sliding fee scale. Use the steps below in patient materials to standardize the application process and make it as easy as possible for them to clearly understand it.
Step 1: Provide applications at the front desk
Direct patients to the front desk to pick up the application or access a digital version. Provide forms in multiple languages where possible.
Step 2: Collect and submit proof of income
Request proof of income such as pay stubs, a tax return, W-2s, Social Security benefit letters, or Medicaid/Medicare documentation. These verify household income and support accurate discount placement.
Step 3: Complete income attestation and consent
Have patients attest to household size and current insurance status, then sign consent for verification. For variable or cash income, accept ledgers, employer letters, or a temporary self-declaration per policy.
Step 4: Offer in-person or digital submission options
Allow an in-person handoff at the front desk, secure upload via portal, or phone assistance for remote applicants.
Step 5: Determine eligibility and assign the discount
Staff should review documents, calculate the percentage of FPL, and confirm eligible patients for the sliding scale fee. Communicate the discount tier and any nominal payment before any scheduling takes place.
Step 6: Reapply annually or when circumstances change
Ask patients to reapply each year or sooner if income, household size, address, or coverage changes.
Tips for common scenarios:
Here are some tips for handling common scenarios that may arise:
- Uninsured patients: Screen for public programs while processing the sliding fee scale. Remember that discounts apply regardless of coverage.
- Medicaid or Medicare recipients: Copy Medicaid/Medicare cards and note how discounts interact with copays or uncovered services.
- Variable or cash income: Accept alternative documentation and a short self-declaration, then schedule a follow-up to confirm updated earnings.
What to expect: Fees and services covered
Under a sliding fee scale, many core healthcare services qualify for reduced charges. Clinics adjust copay, deductibles, and other out-of-pocket amounts by discount tier and document any excluded items.
Use the matrix below during intake and benefits counseling to set clear expectations and align financial assistance policies with sliding scale fee tiers across medical care settings.
| Service category | Examples | Typically covered under a sliding fee scale | Fee notes |
| Primary care visits | New/established visits, chronic care check-ins | Yes | Reduced copay/deductibles by tier. A nominal fee may apply. |
| Behavioral and mental health services | Therapy, counseling, and medication follow-ups | Yes | Session limits may apply. Verify visit length and modality. |
| Dental cleanings and exams | Cleanings, X-rays, simple fillings | Yes | Basic dental services are discounted. Complex procedures may have a higher patient share. |
| Lab tests and basic diagnostics | Blood work, urinalysis, rapid tests | Yes | Advanced imaging (CT/MRI) is often excluded or billed separately. |
| Pharmacy charges | Prescriptions, vaccines at retail pharmacy | No | Pharmacy charges are outside of clinic billing. Consider discount cards or assistance programs. |
| Outside referrals | Specialist visits outside the clinic | No | Not included. Explore charity care or payment plans. |
| Specialty services outside the clinic | Complex procedures, surgeries | No | Not part of the sliding scale fee. Obtain prior cost estimates. |
Tips for providers: Best practices
Every provider offering a sliding fee scale should codify it and train staff across healthcare services to keep access consistent and compliant.
- Document and review policy: Reference the federal poverty guidelines and define income levels, household income, and eligibility. Note how discounts interact with Medicaid, Medicare, and Social Security.
- Align documentation and claims: Standardize intake with EHR software and use electronic claim submission to prevent billing conflicts.
- Communicate access: Post criteria publicly under the health center program, offer multilingual materials, and clarify options for uninsured patients.
- Monitor equity and outcomes: Track utilization, review sliding fee discount program audits, and share improvements that support public health.
Putting sliding fee scales into practice
Sliding fee programs keep healthcare within reach by lowering out-of-pocket costs and expanding healthcare services at your health center. Encourage patients to check eligibility and apply for financial assistance so uninsured patients and underinsured families receive affordable medical care through a clear sliding fee scale and clinic-wide sliding scale fee policy.
Publish criteria on your site, train front desk teams to explain discounts, and offer multilingual materials. When income or household size changes, remind patients to reapply so tiers stay accurate.
For more guidance on your operations, billing, and patient engagement, turn to Tebra as your resource for everything healthcare and healthcare providers.
FAQs
Quick answers to common questions
You might also be interested in
- 5 tips to achieve 100% patient insurance eligibility verification: Enhance your eligibility verification process to reduce claim denials and improve reimbursement rates
- A step-by-step guide to collecting patient payments: Implement effective strategies to streamline patient payment collections and maintain cash flow.
- The ultimate guide to practice automation: Discover how automation can reduce administrative burdens and enhance patient care in your practice.
- Current Version – Nov 20, 2025Written by: Jean LeeChanges: This article was updated to include the most relevant and up-to-date information available.
- Apr 22, 2025Written by: Andrea CurryChanges: This article was updated in 2025 to reflect the latest guidance on sliding fee scales, including eligibility criteria, documentation best practices, and compliance considerations for healthcare providers.







